Community Voices ⎸ Make a plan for end-of-life care
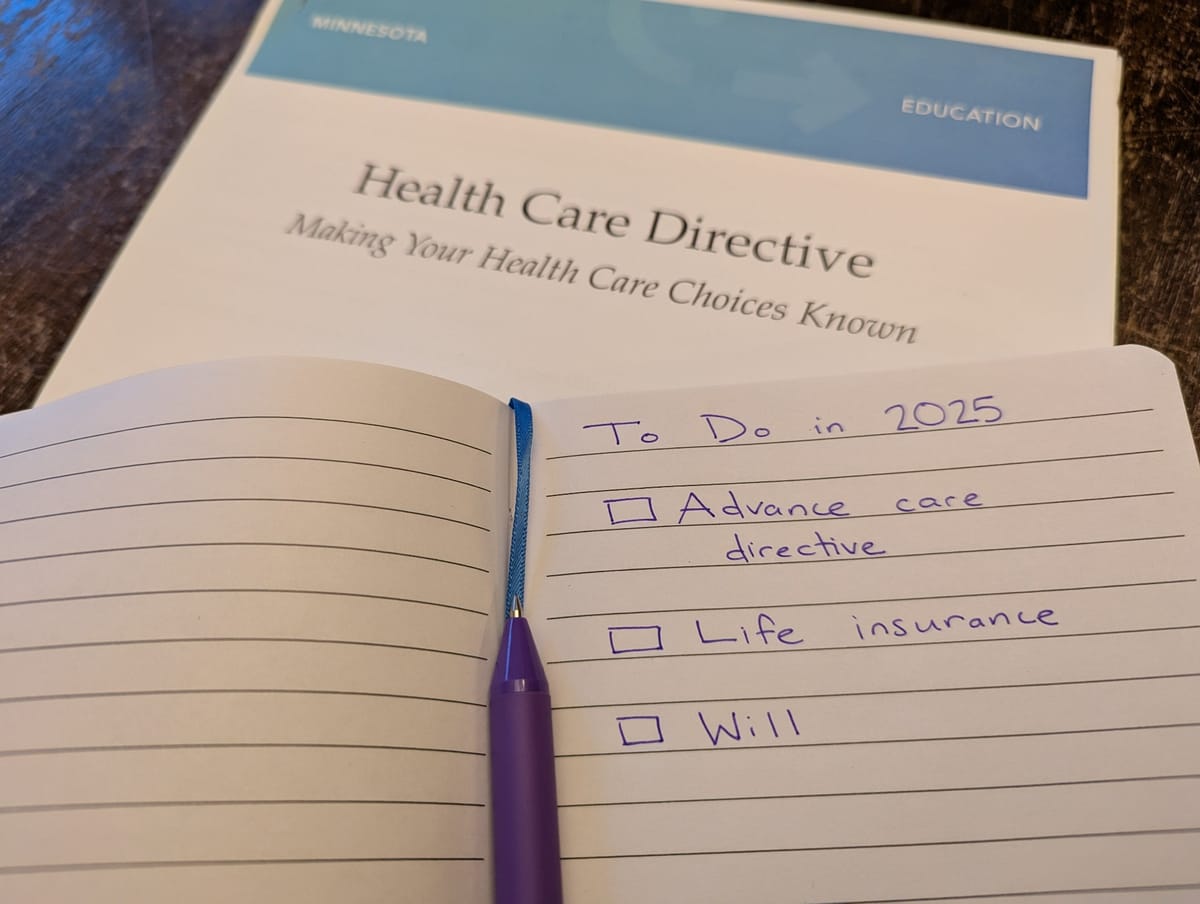
Many Americans don’t have an advance directive. Join the Project Optimist team to make one in 2025.
This story was updated on Feb. 7, 2025, to reflect that more than 210 million Americans do not have an advance care directive or a living will. Project Optimist regrets the error.
Advance directives seem daunting. This year, Project Optimist will demystify them.
About 37% of American adults have an advance care directive and 29% have living wills, according to a 2017 metanalysis published in HealthAffairs. That means more than 210 million American adults aren’t prepared for a serious medical emergency or worst case scenario.
Advance directives let your loved ones and medical professionals know how to care for you if you aren’t able to communicate your wishes, according to the National Institutes of Health.
Sign up for Project Optimist's newsletter
Solution-focused news, local art, community conversations
It's free. No spam. Unsubscribe anytime.
I hadn’t thought about any of this until my dad was diagnosed with brain cancer in 2015. He underwent surgery, went through chemotherapy and radiation, but it wasn’t enough to beat the terminal illness. He started hospice care in January 2017 and died less than two months later.
My dad was stubborn, and like most of us, he was scared about dying. He didn’t want to leave us. He had more to do.
He pushed back when I suggested we go over his will, review his advance care directive, and plan his funeral after he was placed on hospice.
I understood. I didn’t want him to die. I didn’t want to lose him.
But I’m a realist. I didn’t want to wonder what he wanted if he became incapacitated or when he died. I wanted to make sure my brother and I knew.
It’s been almost eight years since he died. My husband and I completed our advance care directives and a will after we had our first child. This year, we’re going to update our will to include our second child.
Project Optimist will run a series on advance care directives throughout 2025 thanks to a grant from the Morgan Family Foundation. This fits with Project Optimist’s focus on news you can use – explanatory reporting and a focus on solutions. This particular solution is preventative and very personal. We want to help demystify it for you.
 Project OptimistJen Zettel-Vandenhouten
Project OptimistJen Zettel-Vandenhouten
Nora Hertel, Project Optimist founder and executive director, and Erica Dischino, Project Optimist’s visual storyteller, will update you each month as they work with their partners to establish advance directives.
If you want to join them, we’re looking for up to five people to make it a 2025 goal and share the process with us. We’ve got some goodies for those who step up!
We’ve also got stories planned on:
- What advanced directives are, how they work, and why they’re important.
- What advance directives look like for Catholics, Somali Americans, and members of the LGBTQ+ community who live in Minnesota.
- Next steps after you’ve got an advance directive in place.
And please let us know if you’d like to share your story with us. Maybe you went through a difficult experience where an advance directive would have been helpful. Let us know how you navigated it. Or maybe you or someone you love put together an advance directive and you can share how the process went. Email me, jen@projectoptimist.news, to share.
This column was edited by Nora Hertel.
It is part of Project Optimist’s series on End-of-Life planning. The series is supported by a grant from the Morgan Family Foundation.
