Community Voices ⎸ Project Optimist staff plan for the end — and it feels good
Life goals: Complete health care directives, draft a will, and enroll in life insurance in 2025.

Visual Storyteller Erica Dischino and Executive Director Nora Hertel will share their journey in 2025 as they “get their affairs in order.” Both have landmark birthdays.
Nora turns 40 and feels behind on these tasks, but, well, adulting is hard. Erica turns 30 and participates to model that it’s really not so painful. They plan to end the year with advance directives (AKA health care directives), wills, and life insurance.
We have prizes for folks who join us on this journey. Email jen@projectoptimist.news if you’re up for it!
Follow along here for an update on their progress each month in 2025. And subscribe to the Project Optimist newsletter for stories about end-of-life planning and how it’s different for different communities and faith groups.
April 1, 2025
• "Answer humanity's ultimate question … no pressure!" by Erica Dischino
• "No tears here" by Nora Hertel
Feb. 25, 2025
• "Find humor in the process" by Erica Dischino
• "I want to feed the flowers" by Nora Hertel
Jan. 28, 2025
• "We start this major adulting challenge" by Erica Dischino
• "One step down, more to go" by Nora Hertel
Project Optimist's End-of-Life series is supported by a grant from the Morgan Family Foundation.
Sign up for Project Optimist's newsletter
Solution-focused news, local art, community conversations
It's free. No spam. Unsubscribe anytime.
April 1, 2025
Answer humanity's ultimate question … no pressure!
By Erica Dischino
Project Optimist
I did it.
After much procrastination, I finally filled out my health care directive. The amount of time I spent thinking about the task far outweighed how long it actually took to complete.
Last month, I spoke with my husband, Mack, about what end-of-life care was important to us. This month, all I had to do was fill the directive out. And man, did I drag my feet on this one.
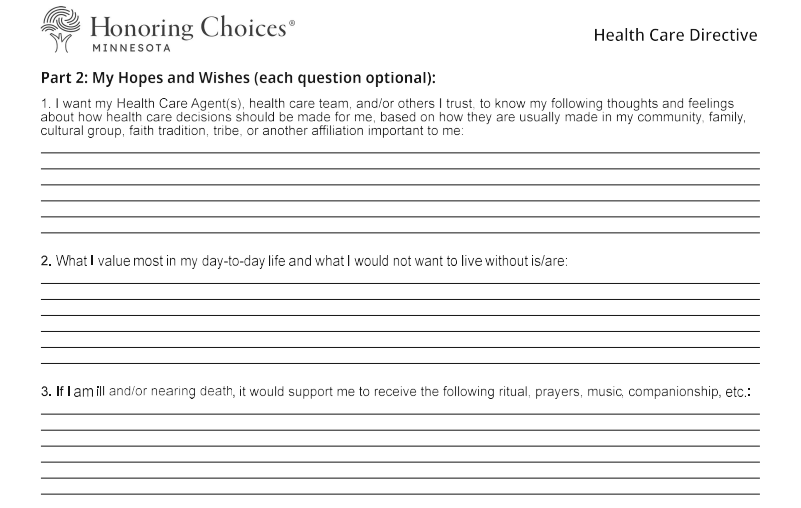
Part of my resistance was having to answer a question in Part 3 of the form, which focused on “My Hopes and Wishes.” In this section, I filled out what I wanted my loved ones to know about “the things that make life most worth living to me.”
How the heck do you know? I can barely choose a dish to order at a restaurant, much less answer the ultimate question of humanity. The amount of music, art, films, plays, and books that have been created trying to answer this question is insurmountable. Of all the things on the directive, this one made my brain explode a bit.
So, I decided to go simple. No poetry, here. I decided the thing that makes life most worth living to me is my relationships. Which means, it’s important to me that I consciously know who I am and who my fellow loved ones are. This is what felt right to me. At least for now.
I’m not sure if I answered the question correctly, but I’ve hopefully got a while to figure it out.
No tears here
By Nora Hertel
Project Optimist
I thought I’d cry my way through this end-of-life project.
I’m a cryer. I recently sobbed through “Little Women.”
But I’ve been laughing (see: February’s update), and sharing in surprising and meaningful conversations.
I asked my spouse to be my health care agent and my sister to be my backup agent. I asked my parents about their plans. After these discussions I feel a new softness where I previously felt tightness in my chest. And a sense of gratitude.
I’ve also talked with two chaplains and a death doula — all people who support people who are dying and their families. These fascinating people aren’t afraid to talk about and experience our most tender, human moments.
We avoid talking about death —or I do —because it’s so tender. But it’s also our most unifying experience. We will all get there. And nearly all of us are afraid to get there. Me too, of course.
In the last three months, as I edited my will and my health care directive, I have found the work to be more gratifying than scary. Softer than I expected.
Have you had conversations with your loved ones about your will or end-of-life wishes? What did you expect? How did it actually go? Let me know: nora@projectoptimist.news.
 Project OptimistJen Zettel-Vandenhouten
Project OptimistJen Zettel-Vandenhouten
February 25, 2025

Find humor in the process
By Erica Dischino
Project Optimist
My husband, Mack, wants to be taxidermied when he dies. More specifically, he wants to be stuffed, then passed down as a family heirloom.
When I told him we needed to have a conversation about end-of-life planning, his lips curled into a facetious grin.
“Well, everything I want is illegal,” he said.
We both cackled. Thinking about death is overwhelming. Every decision feels weighted. But really, the only thing we can do is laugh about it.
I pulled out the health care directive I picked up last month from my doctor’s office.
“OK, one more thing before we start,” he said.
He quickly began playing John Prine’s song, “Please Don’t Bury Me.”
We rifled through the health care directive document that discussed CPR, withholding treatment, and autopsies.
John Prine must’ve selected “yes” to organ donation. I could hear his voice singing:
Please don’t bury me
Down in the cold, cold ground.
No, I’d rather have ’em cut me up
And pass me all around.
Throw my brain in a hurricane,
And the blind can have my eyes,
And the deaf can take both of my ears
If they don’t mind the size.
It’s hard for me to imagine the moment when these decisions will have to be made. Odds are Mack will most likely be the one making them (he is my primary health care agent, now). Checking a box for my own body felt daunting. The thought of Mack having to check a box for me felt like a gut punch.
Preparing for the worst is hard, but having guidance and direct communication with my loved ones makes thinking about my end of life a bit easier.
At least I don’t want to be taxidermied.
 Project OptimistJen Zettel-Vandenhouten
Project OptimistJen Zettel-Vandenhouten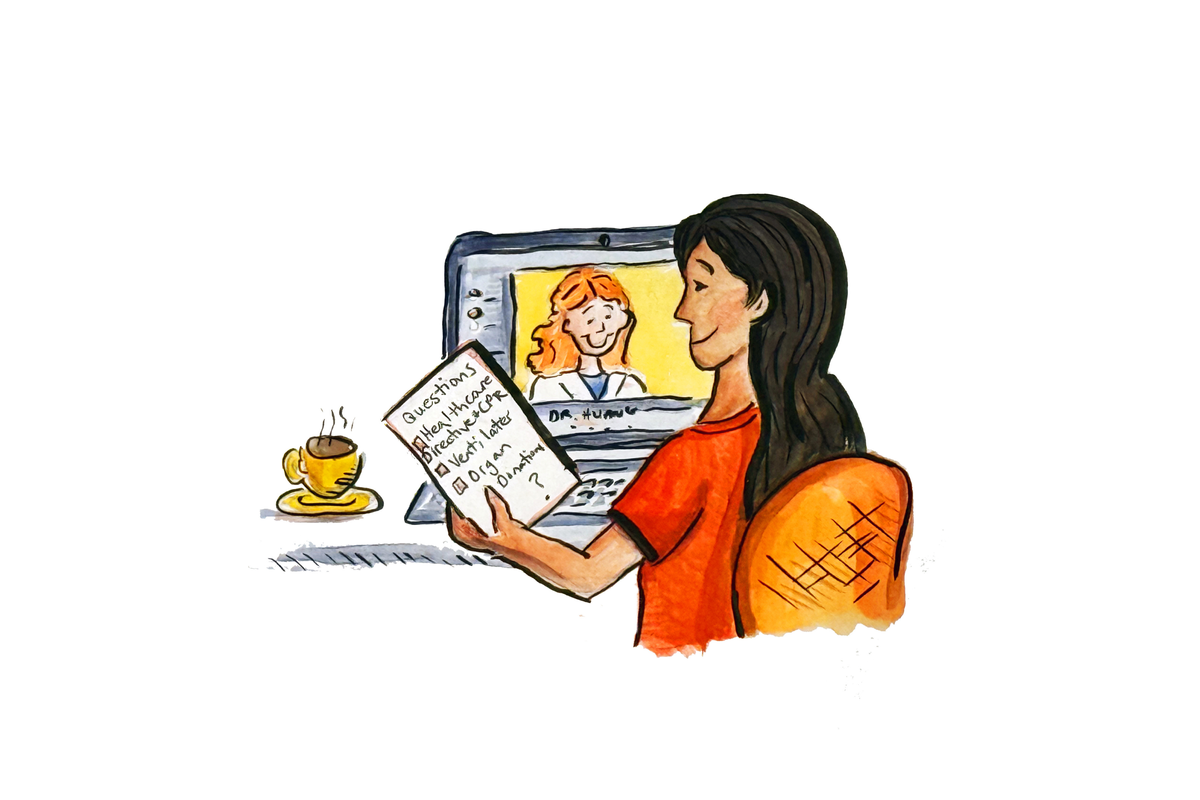

I want to feed the flowers
By Nora Hertel
Project Optimist
I wrote the first draft of my will this week, and I felt a little weird dictating where I’d like my remains to rest when I die.
I’ve been talking about funerals a lot lately because of this project, and it’s brought up some lively conversation and some big laughs. One acquaintance told me his mother-in-law wants to be cremated on a funeral pyre – Viking style.
My preference is for the greenest option. Something that doesn’t release greenhouse gas emissions.
Years ago I listened to a podcast about human composting from Science Vs and found it incredibly moving (so moving in fact that I’ve even imagined making that my next business venture).
If composting is an option when I die, I’ll take it. If it’s not, I vote for a natural burial. I want to give back to the earth that made me.
And it feels good to say so. Now I know that my family and friends don’t have to guess at what I want for my final send-off.
 Project OptimistNora Hertel
Project OptimistNora Hertel
January 28, 2025
We start this major adulting challenge
By Erica Dischino
Project Optimist
My newsfeed tends to highlight the latest trends in diet, exercise, and wellness routines whenever January comes around. The New Year often brings a flurry of hopeful intentions that eventually results in disappointment.
My resolution is a bit different for 2025. Instead of hoping for the best, I’m planning for the worst. And actually, I feel better because of it.
Currently, I’m establishing an advance directive with my husband, Mack. I’ve got a long way to go, but I’ll move slowly and carefully.
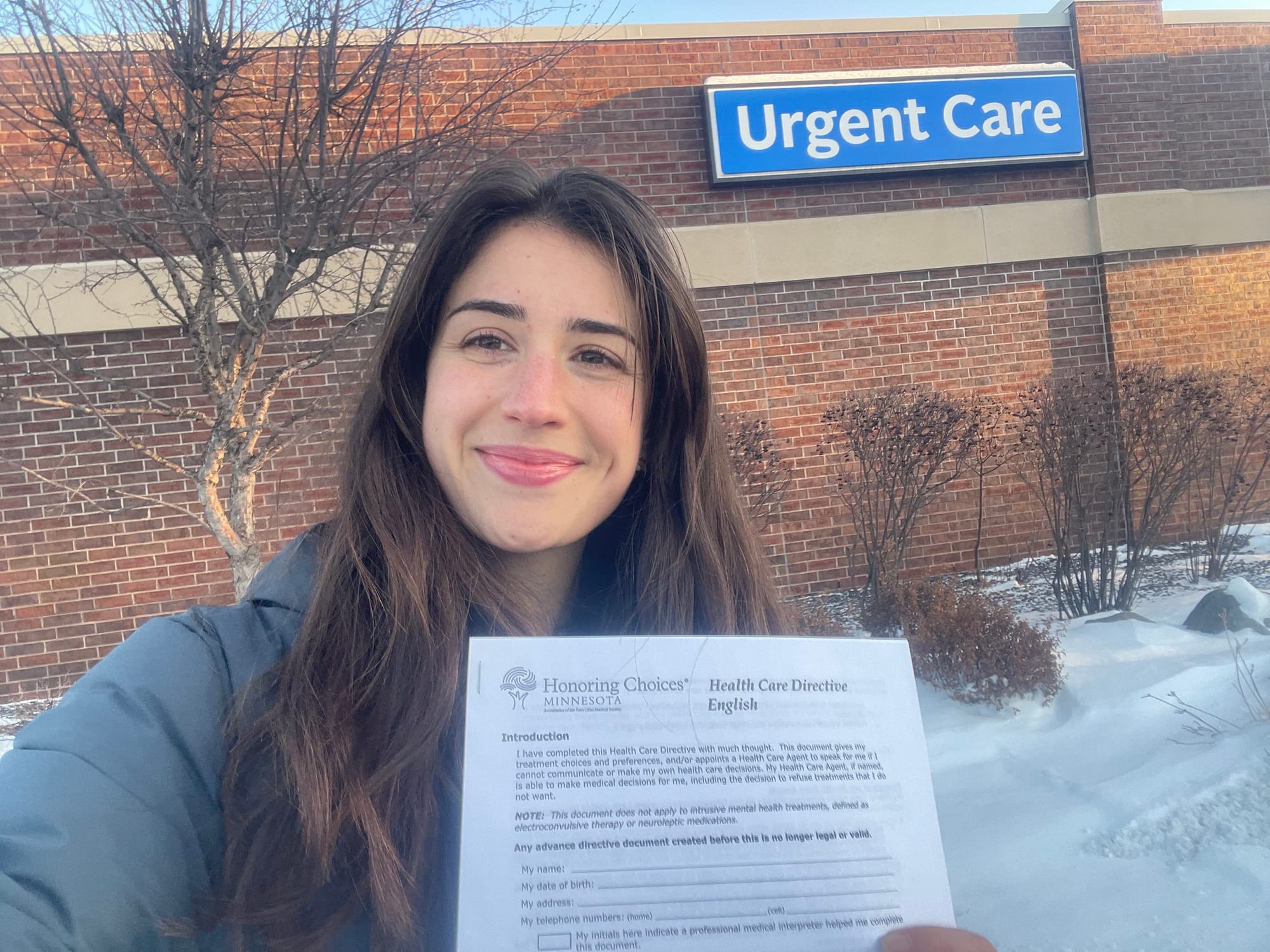
The first step was to head to my local doctor’s office and ask for information.
 Project OptimistJen Zettel-Vandenhouten
Project OptimistJen Zettel-Vandenhouten
I don’t know what motivates you, but going to the doctor’s office to pick up an advance directive information packet is definitely not something that gets me geared up.
I had to do three things to get myself there:
- Tell the Project Optimist team that I was going. I’m a woman of my word!
- Put a reminder on my calendar.
- Get a treat after. My treat was going to the nearby antique store.
Walking in the doctor’s, I felt a bit self-conscious. Am I too young to be doing this? Looking around the room, no one seemed to notice or care. The person at the front desk gave me a packet and voilà, I had done it.
Next up: discuss the information with Mack.
The best form of self-care is preparing yourself and loved ones for when things go wrong. Peace of mind is the greatest wellness hack. I promise you, you won’t be disappointed.
One step down, more to go
By Nora Hertel
Project Optimist
I enter this project with a head start.
I have a legal version of my advance directive that I started and finished THIS MONTH. Proof that it doesn’t require a lot of time or effort.
I had a medical procedure in mid-January that required anesthesia, and the clinic requested my health care directive. I had the form from my doctor’s office. I filled it out over the course of a week. And then I got it notarized at City Hall. Bing, bang, boom.
But it’s not quite right.
 Project OptimistNora Hertel
Project OptimistNora Hertel
I still need to research what happens when someone is on life support. I’m honestly not sure what I want in that situation. When I think of it, I get flashes of sensational TV news sequences about Terri Schiavo. Yes, I’m a child of the ‘90s, and the controversy around Schaivo’s life support stuck in my mind.
I also want to research more to decide if I’d like to donate my body to science.
Then I need to pluck up the courage to discuss all this with my closest family and friends.
My next steps: Research. Get new advance care directive forms for myself and my spouse, Ben. And discuss the document with him.
These blog posts were edited by Jen Zettel-Vandenhouten.
